Introduction
Suicide is a profound public health issue, posing significant challenges to healthcare systems worldwide.

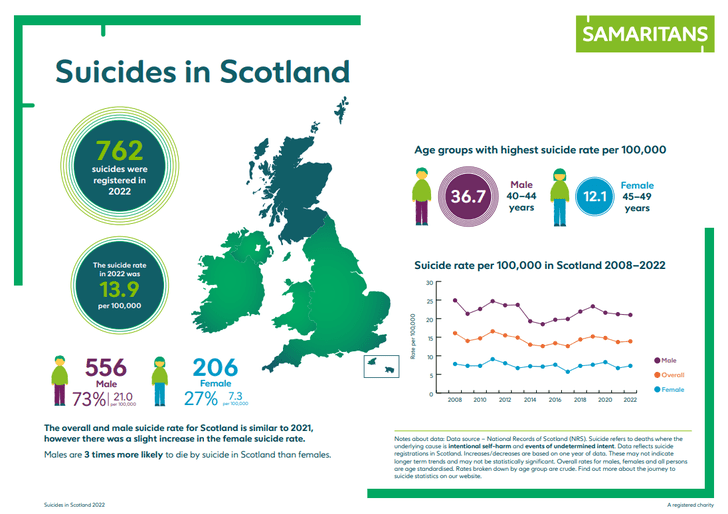
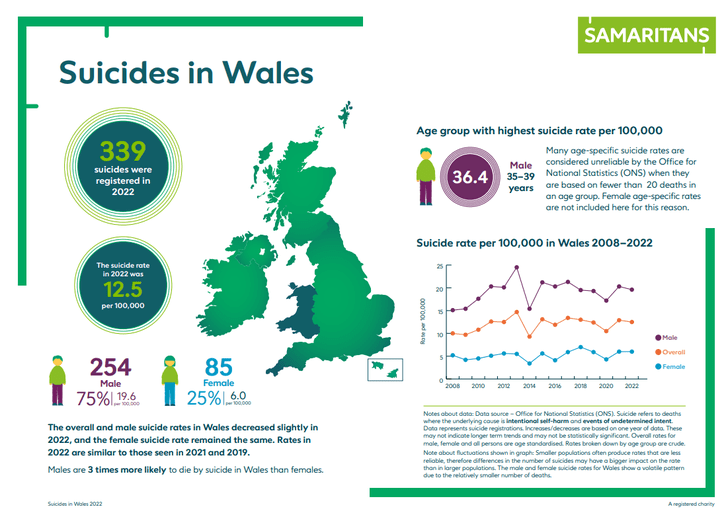
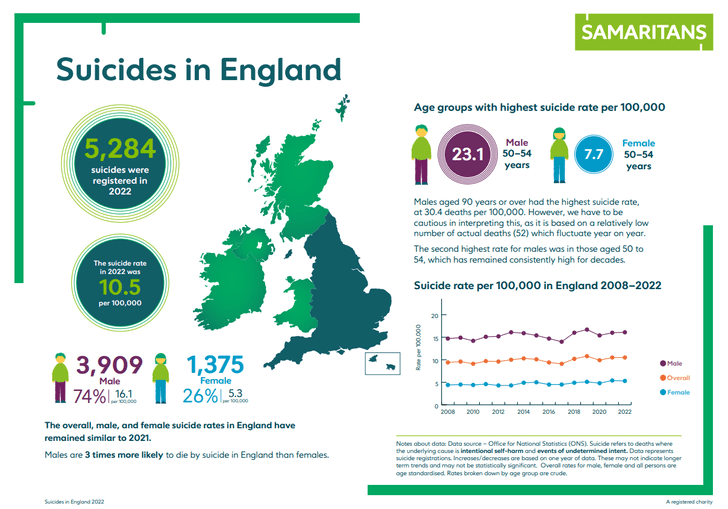
5284 suicides were registered in England in 2022, 339 suicides were registered in Wales 2022, 762 probable suicides were registered in 2022, 203 suicides were registered in Northern Ireland 2022.(Samaritans, 2023)
As the tenth leading cause of death globally, it demands innovative and effective approaches for prevention and intervention. One such approach gaining traction is narrative medicine, which focuses on the importance of patients’ stories in clinical practice. This article explores the potential of narrative medicine to address suicide by enhancing understanding, fostering empathy, and improving patient outcomes.
Understanding Narrative Medicine
Narrative medicine is an interdisciplinary field that integrates the study of literature and the practice of medicine. It emphasizes the importance of understanding patients’ narratives—their personal stories and experiences—in order to provide compassionate and effective care. Originating from the work of Dr. Rita Charon (Charon R. Narrative Medicine: A Model for Empathy, Reflection, Profession, and Trust. JAMA. 2001;286(15):1897–1902.), narrative medicine posits that the act of storytelling can be therapeutic for patients and transformative for healthcare providers. By engaging with patients’ stories, clinicians and professions can gain deeper insights into their experiences, fostering a more holistic approach to care.
The Interconnection of Narrative Medicine and Suicide
Suicide is often the result of complex, multifaceted issues, including mental illness, trauma, social isolation, and existential despair (De Berardis D, Martinotti G, Di Giannantonio M. Editorial: Understanding the Complex Phenomenon of Suicide: From Research to Clinical Practice. Front Psychiatry. 2018 Mar 1;9:61). Traditional biomedical approaches to suicide prevention may not fully address these underlying psychosocial factors. Narrative medicine, however, offers a complementary approach by prioritizing the patient’s voice and personal context.
- Enhancing Understanding through Patient Stories
- Understanding the nuanced experiences of individuals at risk for suicide is crucial. Narrative medicine encourages healthcare providers to listen actively and empathetically to patients’ stories. This process can reveal critical information about patients’ mental states, life circumstances, and coping mechanisms that might not emerge through standard clinical assessments.
- Fostering Empathy and Therapeutic Alliance
- Narrative medicine fosters empathy in healthcare providers through deep engagement with patients’ stories, leading to better understanding of their emotional and psychological pain. This empathy is crucial for forming a therapeutic alliance, essential in effective mental health care, as it encourages patients to express their thoughts and feelings more openly, enabling early intervention and support.
- Identifying and Addressing Biopsychosocial Factors
- Narrative medicine allows for the identification of Biopsychosocial factors that contribute to suicidal ideation. Through storytelling, patients may disclose experiences of trauma, abuse, or significant loss that are pivotal in understanding their mental health struggles. Recognizing these factors enables healthcare providers to tailor interventions that address the root causes of distress rather than just the symptoms.
- Facilitating Healing and Recovery
- The process of narrating one’s story can be inherently therapeutic. It allows individuals to organize their experiences, make sense of their struggles, and find meaning in their lives. For those contemplating suicide, this narrative process can foster a sense of agency and hope. By articulating their stories, patients may begin to see new possibilities for coping and recovery.
Implementation in Clinical Practice
Integrating narrative medicine into clinical practice requires a shift in traditional medical paradigms. It involves training healthcare providers to value and elicit patient narratives and to incorporate these narratives into clinical decision-making. Practical steps include:
- Training Programs: Implementing training programs that teach healthcare providers narrative competence—skills in close reading, reflective writing, and empathetic listening. Engaging healthcare professionals in structured exercises and role-playing scenarios to enhance their understanding and practice of narrative medicine. This approach aims to foster a deeper connection with patients and improve overall quality of care.
- Clinical Settings: Creating clinical settings that encourage storytelling, such as narrative groups or structured interviews that focus on patients’ life stories. Encouraging patients to share their experiences can foster a sense of connection and understanding within the healthcare environment.
- Interdisciplinary Collaboration: Promoting collaboration between medical professionals, mental health specialists, and humanities scholars to enrich the practice of narrative medicine.
Challenges and Future Directions
While narrative medicine shows potential, its incorporation into suicide prevention comes with challenges. These encompass potential time constraints in clinical settings, the requirement for extensive training, and the difficulty in quantitatively measuring the impact of narrative interventions. It is imperative for future research to concentrate on creating standardized protocols for narrative medicine and assessing its efficacy through thorough empirical studies.
Conclusion
Narrative medicine offers a valuable framework for addressing the complex issue of suicide. By prioritizing patients’ stories, it enhances understanding, fosters empathy, and provides a holistic approach to care. While challenges remain, the integration of narrative medicine into clinical practice represents a promising avenue for improving mental health outcomes and preventing suicide. Through continued research and practice, narrative medicine can become a vital component of comprehensive suicide prevention strategies.
Bibliography / Further Reading Suggestions:
- Bajaj, N., Phelan, J., McConnell, E. E. & Reed, S. M. A narrative medicine intervention in pediatric residents led to sustained improvements in resident well-being. Ann Med55, 849–859.
- Cercato, M. C. et al. Narrative medicine: feasibility of a digital narrative diary application in oncology. J Int Med Res50, 03000605211045507 (2022).
- Charon, R. At the Membranes of Care: Stories in Narrative Medicine. Acad Med87, 342–347 (2012).
- Charon, R. The Principles and Practice of Narrative Medicine. (Oxford University Press, 2017).
- Chen, P.-J., Huang, C.-D. & Yeh, S.-J. Impact of a narrative medicine programme on healthcare providers’ empathy scores over time. BMC Med Educ17, 108 (2017).
- Fernandes, I., Martins, C. B. & Reis, A. Creative Dialogues: Narrative and Medicine. (Cambridge Scholars Publishing, 2015).
- Fioretti, C. et al. Research studies on patients’ illness experience using the Narrative Medicine approach: a systematic review. BMJ Open6, e011220 (2016).
- Fox, D. A. & Hauser, J. M. Exploring perception and usage of narrative medicine by physician specialty: a qualitative analysis. Philos Ethics Humanit Med16, 7 (2021).
- Fox, D. A. & Hauser, J. M. Exploring perception and usage of narrative medicine by physician specialty: a qualitative analysis. Philos Ethics Humanit Med16, 7 (2021).
- Guo, T., Sun, Y. & Li, G. Knowledge, Attitude, and Practice regarding Narrative Medicine among Chinese Medical Personnel: An Online Cross-Sectional Survey. Comput Math Methods Med2022, 3329360 (2022).
- Huang, C.-D. et al. How does narrative medicine impact medical trainees’ learning of professionalism? A qualitative study. BMC Med Educ21, 391 (2021).
- Huang, Y., Monrouxe, L. V. & Huang, C.-D. The influence of narrative medicine on medical students’ readiness for holistic care practice: a realist synthesis protocol. BMJ Open9, e029588 (2019).
- Liao, H.-C. & Wang, Y.-H. Narrative medicine and humanities for health professions education: an experimental study. Med Educ Online28, 2235749.
- Liao, K.-C. et al. Understanding the lived experiences of medical learners in a narrative medicine course: a phenomenological study. BMC Med Educ21, 321 (2021).
- Marini, M. G. Narrative Medicine: Bridging the Gap between Evidence-Based Care and Medical Humanities. (Springer, 2015).
- Meza, J. P. & Passerman, D. S. Integrating Narrative Medicine and Evidence-Based Medicine: The Everyday Social Practice of Healing. (Radcliffe Publishing, 2011).
- Remein, C. D. et al. Content and outcomes of narrative medicine programmes: a systematic review of the literature through 2019. BMJ Open10, e031568 (2020).
- Robertson, C., Clegg, G. & Huntley, J. Storytelling in Medicine: How Narrative Can Improve Practice. (CRC Press, 2023).
- Surgeons, R. C. P. of C. M. C. U. C. of P. and. Narrative Medicine : Honoring the Stories of Illness: Honoring the Stories of Illness. (Oxford University Press, USA, 2006).


Leave a comment