Neurodiversity, Suicide, and Occupational Health in Scotland – SOM Conference
Recently I delivered this talk as a guest of the Society of Occupational Medicine, the given talk included a number of personal anecdotes which are not included here.
I’m Dr. Simon Harold Walker, Senior Research Lead at the Healthy Working Lives Group at the University of Glasgow. My focus spans occupational health, neurodivergence, and suicidology—areas often discussed in silos but that critically intersect in Scotland.

Today, I’ll dive into how these intersections impact the well-being of neurodivergent individuals in the workplace and beyond, and why we need to address the gaps in understanding suicide risk within these populations.

First, I want to quickly give a pitch for RESUME.
The RESUME project, REsearch into Scottish nursing SUicide and Mental health Experiences, is an interdisciplinary study aiming to address the elevated suicide risk and mental health challenges faced by nursing professionals in Scotland between 1980 and 2025. Combining qualitative interviews with quantitative analysis of national datasets, RESUME identifies key risk factors—such as workplace trauma, personal crises, and job role-related stress—that contribute to mental health struggles in this demographic. Key partnerships include NHS Scotland, the Royal College of Nursing Scotland, and the Queen’s Nursing Institute Scotland. These collaborations support participant recruitment, access to historical data, and the application of insights into policy and intervention development within the healthcare system.
RESUME also involves the development of a predictive algorithm designed to help workplaces identify at-risk individuals more effectively, enhancing proactive intervention capabilities. In addition, the project features the ASC app, which provides real-time mental health support specifically for nurses, aiming to foster improved intervention strategies and ultimately reduce suicides within the nursing profession in Scotland.
Neurodiversity isn’t just a trendy term; it’s the recognition that cognitive differences—like autism, ADHD, and dyslexia—are natural variations, not deficits. Neurodivergent individuals process information differently, which is as biologically rooted as height.
However, unlike height, these differences are often stigmatized or poorly understood, especially in workplaces that still default to “one-size-fits-all” practices. This fundamental lack of adaptation and understanding in occupational settings is a significant contributor to the mental health challenges and isolation that many neurodivergent employees face (Scottish Government, 2021).

Neurodivergent individuals are at increased risk of anxiety, depression, and other mental health issues. Statistics reflect a concerning trend: studies show that 34.2% of autistic individuals experience suicidal ideation, significantly higher than in neurotypical populations (Autistica, 2018). ADHD carries a similarly high risk, with a 2019 meta-analysis linking it to suicide attempts at nearly twice the rate of the general population (Papyrus UK, 2022). These vulnerabilities make it imperative that we rethink mental health support systems in ways that reflect the unique needs of neurodivergent individuals, particularly in occupational settings where these stressors often peak.
Occupational settings can be particularly challenging for neurodivergent individuals, who often experience heightened stress due to lack of accommodations, misunderstanding from colleagues, and pressure to mask their differences. The link between neurodivergence and suicide is underscored by studies showing elevated suicide rates among neurodivergent populations. For example, people with dyslexia face a higher risk of depression and anxiety, both of which correlate strongly with suicidality. Yet, here in Scotland, our reporting systems lack the granularity to track neurodivergent status in suicide cases, making it difficult to develop targeted support and prevention strategies. In this sense, we’re fighting blindfolded, unable to fully understand the scope of the issue or develop proactive interventions.

The Equality Act 2010 requires Scottish employers to make reasonable adjustments for disabled employees, a mandate that extends to many neurodivergent individuals. But compliance is often minimal and inconsistent. Neurodivergent employees face barriers from physical workspace layout to sensory overload and rigid communication styles, which occupational health practitioners could help to alleviate—if they’re trained to recognise and address these needs. Many employers still see occupational health as a box-ticking exercise rather than an avenue to foster true inclusivity. This lack of real engagement leads to burnout, mental health decline, and, tragically, suicide for some neurodivergent individuals (Scottish Government, 2021).
Neurodivergent employees face challenges that neurotypical colleagues may rarely consider. Sensory sensitivities, difficulty with social cues, and the cognitive load required to “mask” neurodivergent traits can be exhausting. Nearly 40% of Scottish workers report that workplace stress impacts their mental health (Scottish Government Mental Health Strategy, 2022), and for neurodivergent employees, these issues are amplified. They often find themselves choosing between risking their mental health by masking or risking their careers by being their authentic selves—both paths fraught with consequences.
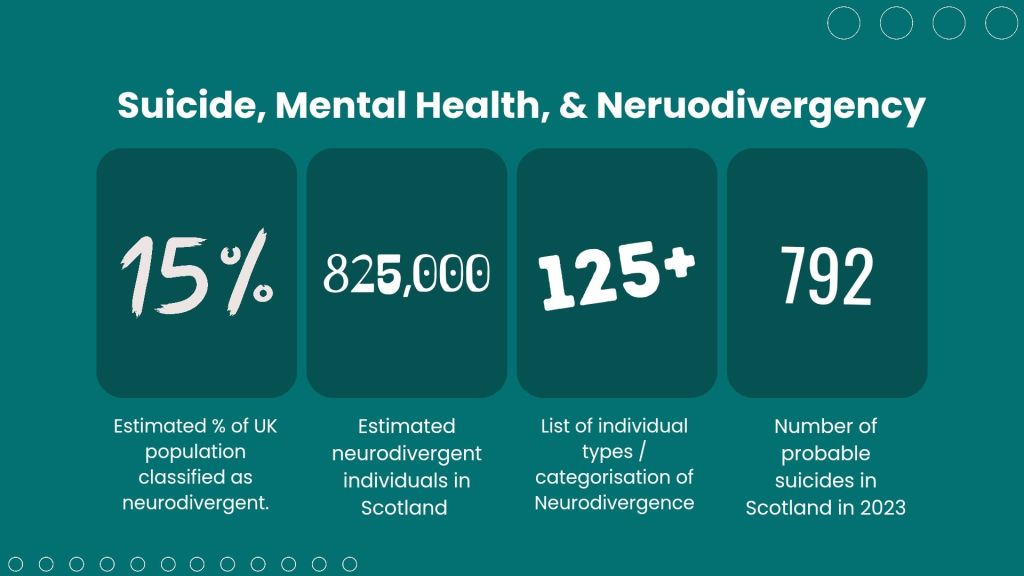
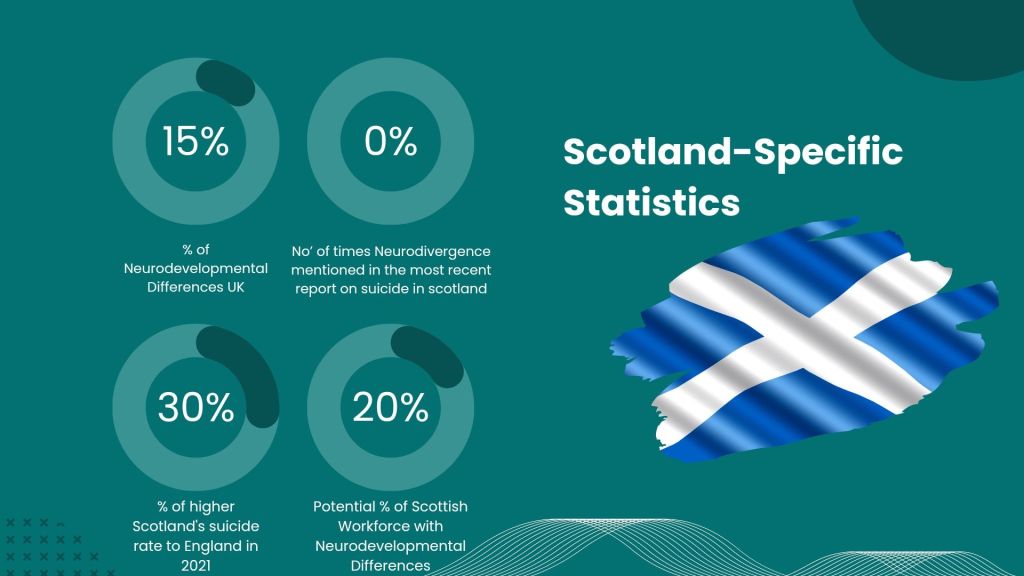
In the UK, an estimated 15-20% of the population is neurodivergent, translating to roughly 825,000 individuals in Scotland alone (Mental Health Foundation, 2023). Scotland has a suicide rate about 15% higher than England’s, with 792 probable suicides recorded in 2023 (National Records of Scotland, 2023). However, we don’t have reliable data linking neurodivergent status to suicide cases. The absence of this data hampers our ability to craft policies and interventions that could potentially save lives. We must advocate for suicide tracking that includes neurodivergent identifiers, enabling us to understand and address this intersection of risk more effectively.

Occupational health plays a unique role in reducing suicide risk. Proactive assessments and workplace accommodations—such as sensory-friendly environments or flexible schedules—could provide neurodivergent employees with the stability they need to thrive. Research by Autistica (2018) highlights that tailored workplace adjustments can significantly decrease suicide risk by reducing stress factors that impact neurodivergent individuals more severely than their neurotypical peers. It’s clear that an investment in inclusive occupational health practices is also an investment in suicide prevention.
Stigma, lack of awareness, and insufficient training among managers are pervasive barriers. These obstacles make it difficult for neurodivergent employees to access mental health resources or seek accommodations. Without targeted support, neurodivergent employees face an uphill battle, often resulting in mental health deterioration and an increased suicide risk. Occupational health practitioners are ideally positioned to lead the way in changing this dynamic, provided they have the right training and resources.
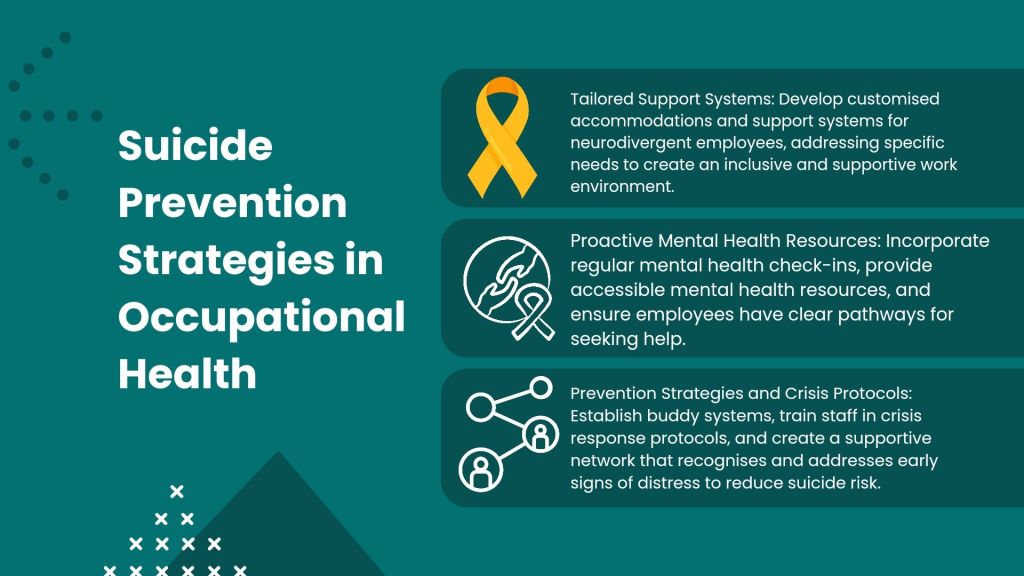
Key strategies include:
Tailored Support Systems: Occupational health practitioners should develop customised accommodations and support systems to create a workplace where neurodivergent employees feel understood and valued.
Proactive Mental Health Resources: Employers should offer regular check-ins, accessible mental health resources, and clearly communicated pathways for seeking help.
Crisis Protocols and Prevention Strategies: Implementing buddy systems, training staff in crisis response, and creating supportive networks can help detect and address early signs of distress, reducing suicide risk.

While the Equality Act 2010 and the Mental Health (Care and Treatment) (Scotland) Act 2003 set foundational protections, more is needed. The proposed Learning Disabilities, Autism, and Neurodivergence Bill aims to bridge the gaps, offering additional protections and workplace support. This legislation represents a step forward, but its success hinges on real commitment from occupational health practitioners, employers, and policymakers to ensure that neurodivergent employees have meaningful, consistent support.

Occupational health practitioners in Scotland are key to identifying and mitigating suicide risk among neurodivergent employees. Practitioners can conduct proactive assessments, recommend reasonable adjustments, and educate employers on the unique stressors that neurodivergent employees face. Through these actions, they align with Scotland’s broader initiatives for inclusivity and mental well-being, fostering workplaces where neurodivergent individuals feel safe, supported, and able to thrive.

Raising awareness around neurodiversity in occupational health is critical for reducing suicidality among neurodivergent individuals. An inclusive approach—where workplace accommodations are normalised, mental health resources are accessible, and individuals feel supported—can transform the workplace into a space that nurtures rather than endangers mental health. Scotland has the legislative framework to make this a reality; what’s needed now is action from occupational health practitioners and employers to bring these protections to life. Only then can we hope to create safer, more resilient workplaces for everyone.



Leave a comment